Blog
Illuminating the Science of Cannabis Schizophrenia: Latest Research on Cannabis and its Potential Impact on Mental Health
In recent years, the topic of cannabis and its potential impact on mental health, particularly schizophrenia, has been a subject of intense scientific inquiry and public interest. Cannabis, commonly known as marijuana, is one of the most widely used psychoactive substances worldwide, and its legalization in several regions has sparked discussions about its potential benefits and risks. As researchers delve deeper into the relationship between cannabis and schizophrenia, it becomes evident that the matter is far more complex than previously thought. This magazine-style blog aims to shed light on the latest scientific research concerning cannabis and its potential impact on schizophrenia. From the role of cannabinoids to the influence of genetics, we embark on an illuminating journey to understand the nuances of this intriguing relationship.
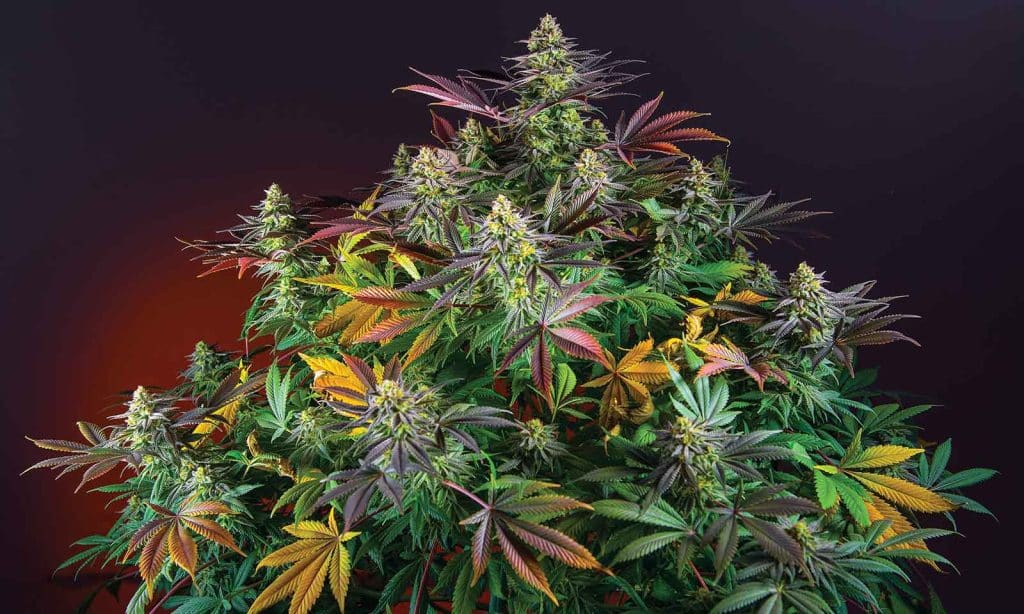
Unraveling the Cannabis Plant: Cannabinoids and Beyond

To comprehend the potential impact of cannabis on schizophrenia, we must delve into the intricate composition of the cannabis plant. This versatile plant contains a myriad of chemical compounds known as cannabinoids, each with unique properties and effects on the human body. Among these cannabinoids, tetrahydrocannabinol (THC) and cannabidiol (CBD) take center stage in discussions surrounding Cannabis Schizophrenia. THC, abundant in certain cannabis varieties, is notorious for its psychoactive properties, responsible for the characteristic “high” experienced by recreational users. However, THC’s relationship with schizophrenia is more complex. Emerging research suggests that THC’s interaction with the brain’s endocannabinoid system, a complex network of receptors involved in various physiological processes, might contribute to the onset and progression of schizophrenia symptoms in vulnerable individuals.
On the other hand, CBD, another prominent cannabinoid found in the cannabis plant, has garnered considerable attention for its potential therapeutic benefits without inducing intoxication, making it a compelling subject in the realm of Cannabis Schizophrenia. CBD’s non-psychoactive nature has led to its exploration as a potential antipsychotic agent. Studies investigating the effects of CBD on schizophrenia have shown promising results, with evidence suggesting that CBD might have an impact on mitigating psychotic symptoms associated with the disorder. Its antipsychotic potential lies in its interactions with different receptors, neurotransmitter systems, and other signaling pathways in the brain, indicating a multifaceted approach to modulating mental health.
Understanding the dynamic interplay between THC, CBD, and other cannabinoids within the cannabis plant is a crucial step in comprehending cannabis’s potential impact on schizophrenia. Researchers are working tirelessly to uncover the complex mechanisms behind the interplay between these compounds, shedding light on their individual effects and the collective influence they exert on the human brain concerning Cannabis Schizophrenia. As the scientific community delves deeper into the intricate world of cannabinoids and their impact on mental health, we can hope to gain valuable insights that will inform responsible cannabis use and contribute to the development of targeted interventions for individuals with schizophrenia.
The Schizophrenia-Cannabis Conundrum: Is There a Causal Link?
The relationship between cannabis use and schizophrenia is a topic that has captured the attention of researchers and healthcare professionals alike. While numerous epidemiological studies have found a correlation between cannabis use and an increased risk of developing schizophrenia, establishing causality remains a challenging task. The complexity of this conundrum arises from the interplay of various factors, including genetics, environment, and individual vulnerability.
One school of thought posits that individuals with a genetic predisposition to schizophrenia may be more likely to use cannabis as a form of self-medication to alleviate early symptoms or distress. This self-medicating behavior could potentially explain the observed association between cannabis use and schizophrenia risk in some individuals, known as the Cannabis Schizophrenia conundrum. On the other hand, an opposing viewpoint suggests that cannabis use may, in fact, trigger or exacerbate schizophrenia in vulnerable individuals. According to this perspective, cannabis use, particularly in adolescence when the brain is still developing, may interact with specific genetic factors and environmental influences to increase the likelihood of developing schizophrenia in those already at risk.
To resolve this complex issue, rigorous longitudinal studies are necessary to disentangle causality from correlation within the context of Cannabis Schizophrenia. Long-term investigations that follow individuals over extended periods can help identify temporal relationships between cannabis use and the onset of schizophrenia symptoms. Additionally, the examination of potential risk factors associated with cannabis use and schizophrenia, such as the age of initiation, frequency of use, and THC potency, is essential for a comprehensive understanding of the relationship.
The conundrum also underscores the importance of personalized medicine and precision psychiatry concerning Cannabis Schizophrenia. Individuals may respond differently to cannabis use based on their genetic makeup, and identifying these genetic variations can aid in identifying those who may be more vulnerable to the potential effects of cannabis on schizophrenia.
The question of whether there is a causal link between cannabis use and schizophrenia remains a topic of debate within the scientific community, especially in the context of Cannabis Schizophrenia. The complex interplay of genetic, environmental, and individual factors adds layers of intricacy to this relationship. While the correlation between cannabis use and schizophrenia risk is evident, rigorous and long-term studies are needed to establish causality definitively concerning Cannabis Schizophrenia. As we advance in understanding the mechanisms behind this conundrum, healthcare professionals must emphasize evidence-based education and targeted interventions to inform individuals about potential risks and promote responsible cannabis use, particularly in those with predispositions to mental health conditions like schizophrenia.
Unraveling the Genetics: Gene-Environment Interactions
The field of genetics has long been recognized as a significant contributor to the development of schizophrenia, a complex neuropsychiatric disorder characterized by a range of symptoms, including hallucinations, delusions, and impaired cognitive function. However, the intricate interplay between genetic factors and environmental exposures, such as cannabis use, has introduced a new dimension of complexity in our understanding of this condition. Researchers have identified certain genetic variations, such as specific gene variants, that are associated with an increased risk of developing schizophrenia. These genetic factors can influence various neurobiological processes and pathways, potentially making individuals more susceptible to the disease.
As the scientific community delves deeper into the relationship between cannabis and schizophrenia, studies are now exploring how cannabis use may interact with these genetic factors to modulate the expression of the disease. It is hypothesized that cannabis’s impact on the brain’s endocannabinoid system, particularly the influence of THC, may interact with specific genetic variants associated with schizophrenia, either triggering the onset of the disorder or exacerbating its symptoms in vulnerable individuals.
Studying gene-environment interactions in the context of schizophrenia and cannabis use can offer valuable insights into personalized risk assessment. By identifying individuals who may be more susceptible to the potential impact of cannabis on schizophrenia due to their genetic makeup, healthcare professionals can tailor interventions and preventive measures accordingly. This targeted approach may involve offering counseling and education about the potential risks of cannabis use to individuals with specific genetic risk factors for schizophrenia. It also emphasizes the importance of early intervention and monitoring for individuals who have a genetic predisposition to the disorder and engage in cannabis use.
Understanding gene-environment interactions can inform the development of precision medicine approaches for schizophrenia management. By identifying specific genetic markers associated with a positive response to certain treatments, researchers can develop personalized treatment plans for affected individuals. Additionally, studying these interactions may shed light on potential mechanisms through which cannabis influences the expression of schizophrenia-related genes, offering new targets for drug development and therapeutic interventions.
It is important to note that the relationship between cannabis use and schizophrenia is complex and multifaceted. While genetics plays a crucial role, environmental factors, such as stress, trauma, and substance use, also contribute to the development of schizophrenia. The interplay between genetic predisposition and environmental exposures adds layers of complexity that necessitate rigorous scientific investigations.
Overall, unraveling the genetics of schizophrenia and the gene-environment interactions with cannabis is a dynamic and evolving field of research. It holds promise for advancing our understanding of the disease’s etiology and may pave the way for more targeted and personalized approaches to schizophrenia prevention and management. However, as research progresses, it is essential to approach the findings with caution and recognize the need for further studies to validate and expand upon these preliminary insights. Ultimately, a comprehensive and multidisciplinary approach that integrates genetics, neuroscience, and environmental factors will be key to advancing our knowledge and improving outcomes for individuals affected by Cannabis Schizophrenia.
Navigating the Clinical Implications: Cannabis-Based Therapies for Schizophrenia

As the scientific community continues to delve into the intricate relationship between cannabis and schizophrenia, the potential of cannabis-based therapies for managing schizophrenia has captured the attention of researchers and medical professionals alike. In recent years, clinical trials have been initiated to investigate the therapeutic effects of cannabidiol (CBD) as an adjunct treatment for schizophrenia. CBD, a non-psychoactive compound found in the cannabis plant, has shown promise in mitigating psychotic symptoms and improving overall mental well-being in individuals with schizophrenia. These studies exploring the effects of cannabis on schizophrenia present promising avenues for future treatment options, and it is essential to carefully examine the potential benefits and risks associated with cannabis-based therapies for schizophrenia management. Addressing standardized dosing is critical in determining the optimal CBD dosage for schizophrenia patients, taking into account individual responses and potential interactions with other medications to ensure personalized care. Furthermore, comprehensive, long-term studies are necessary to better understand the long-term safety profile of cannabis-based treatments, particularly for individuals with schizophrenia. By exploring the variability in individual responses to cannabis-based therapies, researchers can tailor treatment plans and maximize the benefits for each patient’s unique needs. As the field of cannabis schizophrenia research continues to evolve, collaboration between researchers, clinicians, and patients is vital in responsibly navigating the clinical implications of cannabis-based therapies for schizophrenia management and providing individuals with a range of safe and effective treatment options to enhance overall well-being and symptom management.
Unraveling the Complex Connection
The exploration of cannabis and its potential impact on schizophrenia is a multifaceted endeavor that requires a balanced and evidence-based approach. As the latest scientific research continues to illuminate this intricate relationship, it becomes evident that cannabis’s impact on schizophrenia is influenced by a complex interplay of cannabinoids, genetic factors, and environmental exposures. Researchers and healthcare professionals must collaborate to ensure the responsible dissemination of information to the public, promoting awareness of potential risks and benefits. By fostering a deeper understanding of cannabis and schizophrenia, we can pave the way for informed decisions, targeted interventions, and advancements in mental health care, ultimately enhancing the well-being of individuals affected by this complex neuropsychiatric disorder.